COVID-19 Evaluation and Management
This is designed to be a quick rundown of COVID-19 and a suggested format to use when working up patients (From an ED perspective) with various levels of acuity and presentation based on literature to date and multiple sources.
Predominant symptoms of COVID-19 consist of fever (90%), cough and dyspnea (61-86%) with anosmia, dysgeusia, diarrhea, sore throat and myalgias (18-50%). Less frequently but still seen are chest pain, altered mental status (6-15%). Commonly GI symptoms may precede upper respiratory symptoms and in many cases isolated fever without other symptoms is common. 43% of COVID-19 infections are reportedly asymptomatic. (1,20)
General COVID DDx: Influenza, sepsis, PNA/bronchitis, electrolyte abnls, infectious GI conditions, MI, PE, stroke, microvascular complications. Also consider COPD/CHF.
Typical lab findings:
– Lymphocytopenia (80%)
– hypoalbuminemia (50-98%)
– Elevated inflammatory markers –> LDH, Ferritin, Dimer, CRP, ESR, neutrophils, wbc.
– less seen but still possibly elevated –> Trop, sCr, CK. (19)
General stuff
COVID seems to peak around days 7-11 in terms of severity. At this stage typically patients start to progress and get better symptomatically or decline and develop respiratory insufficiency.
COPD and asthma do not seem to increase propensity to develop COVID, and are not typically correlated with worse prognosis. (3) Don’t avoid steroids like Prenisone/prednisolone for these patients – if they need it, give it.
COVID can cause atypical clotting and microvascular thrombosis, MI and PE’s have been seen, typically in sicker patients, although don’t discount this in hypoxic patients without additional symptoms.
CXR and imaging typically will show ground glass opacities and infiltrates in a bilateral distribution. CT similar pattern. A negative CXR is no guarantee that COVID-19 infection is not present. (16)
Procalcitonin not typically very elevated in COVID only patients. If underlying or superimposed bacterial process – will likely be more elevated (>1.0).
Decompensation in COVID is unpredicatable–> even well appearing/minimal Risk factor patients can decompensate and require escalation of care. If they are discharged they should be given strict return precautions and possibly consider home SPO2 monitoring dependent on RF. (17)
Fluids –> initial consensus was fluid restrictive (Makes sense for true ARDS) however if the patient requires resuscitation and/or has renal failure or other need for fluid administration, they can receive some IVF. (Don’t run them completely dry). But don’t be overzealous with IVF either as this condition carries a risk of “acquired volume overload”. Judicious use is the key. (15)
Stroke and MI are complications of COVID-19. If you have these type of patient presentations consider investigating for underlying COVID and possible anticoagulation strategies if suspected microvascular complications.
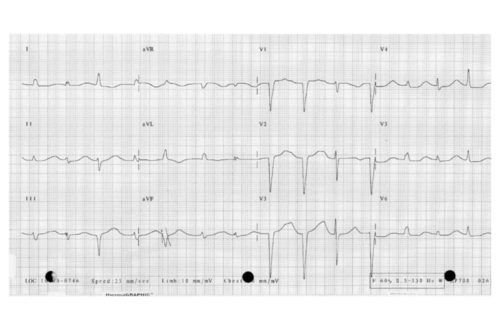
Troponinemia may be seen for multiple reasons –> True ACS, or Type II process with strain from viral or bacterial infection. Need ASA and consider anticoagulation strategies per JACC (18). If possible myocarditis –> Supportive care but ICU level care. According to JACC –> PCI still standard of care for STEMI patients with COVID-19 (5).
Workups – Lets talk acuity
The Low Acuity patient – 0-7 days of symptoms, normal vitals (aside from some mild tachycardia or fever, and normoxic (SPO2 97-100%).
- no/minimal co-morbidities and risk factors –> treat symptoms – antipyretics, supportive care. General imaging and labs typically not required.
- some co-morbidities –> CXR, cbc, cmp, eval electrolyte disturbances, AKI etc.
- Generally the above patients are stable for dc with strict return precautions.
- Multiple co-morbidities –> Consider expanding workup with xray, EKG, ferritin/LDH/Dimer/CRP/Procalcitonin. Dispo –> Observation admission vs Home SPO2 monitoring. These patients are higher risk for decompensation
The Moderate Acuity patient – 0-21 days of symptoms, HR >115, mild hypoxia (SPO2 92-97%). Return or recurrent presentations carry higher risk.
- no/minimal comorbidities –> Consider full workup with xray, EKG, Trop, ferritin/LDH/Dimer/CRP/Procalcitonin. Dispo –> home with SPO2 monitoring and supplemental O2 vs Observation admission depending on patient tolerance.
- multiple comorbidities –> Full workup with xray, EKG, Trop, ferritin/LDH/Dimer/CRP/Procalcitonin. Dispo –> Medical observation/admission.
- These patients benefit from NC O2 4-15L (NRB or AIRVO) if needed, self proning/decubitus positioning for recruitment and pulmonary blood flow strategies while in the ED.
- I don’t typically obtain blood gas for these patients unless continued or progressive hypoxia with supplemental O2. In that case PE evaluation may be indicated.
- consider lovenox 1mg/kg or UFH for these patients to reduce microvascular thrombotic complications if admitting
The High Acuity patient –> 0-21 days or symptoms, or return after prior infection/hospitalization, “silent” or symptomatic hypoxia (SP02 <90%), Tachycardia HR>115.
- Full workup with xray, EKG, Trop, ferritin/LDH/Dimer/CRP/Procalcitonin/blood gas/lactate. I also add blood cultures x2, and consider Abx (as below) if they have elevated procalcitonin and possible superimposed infection –> Ceftriaxone+ Doxycycline for CAP coverage, Vanc+Cefepime for VAP/HAP/HCAP coverage –> Vanc +Cefepime +Tobramycin for MDR Pseudomonas risk. (Consider patient RF ie Prior ICU stay etc –>Consult pharmacy).
- Streptococcus pneumoniae, Klebsiella pneumoniae, and Haemophilus influenzae were the most common superimposed bacterial respiratory co-infections in a large study (4).
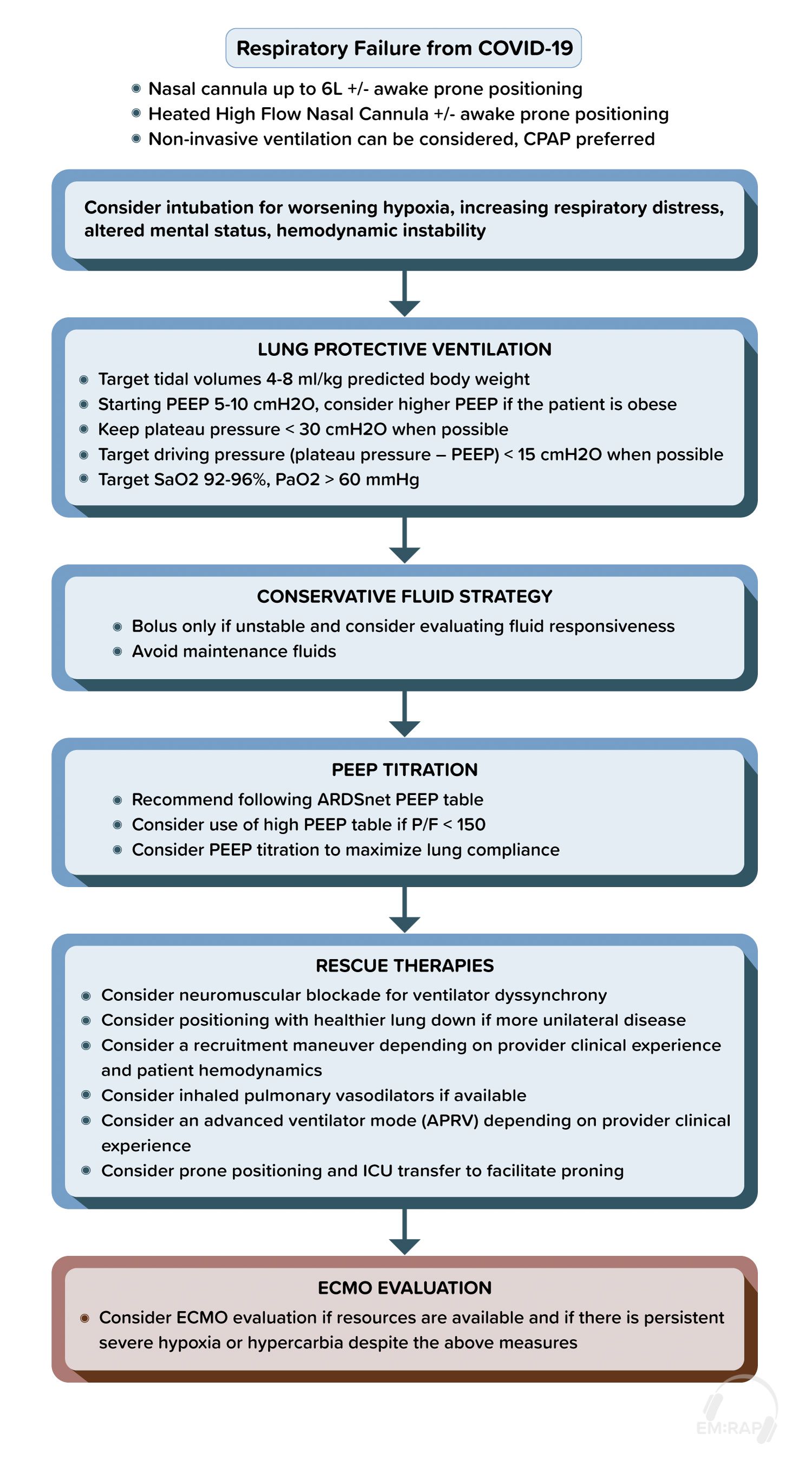
- Lung preservation strategies –> AIRVO/BiPAP/CPAP/NPPV as much as possible – try to avoid intubation until inevitable as this seems to cause pulmonary and alveolar damage, pulmonary scarring, and ventilatory support possibly is an inciting factor in cytokine storm.
- If unable to avoid intubation (AMS, significant respiratory fatigue, shock, progressive acidosis or hypercarbia etc) –> Intubation with ARDSNet lung protective strategy –> 4-8cc/kg TV, low PEEP (5ish), low plateau pressures where possible (<30 mmh20). SPO2 goal of 92% or higher if possible.
- These patients qualify for Dexamethasone and Remdisivir administration depending on protocol.
- lovenox 1mg/kg or UFH for these patients to reduce microvascular thrombotic complications
- If significant hypoxia and elevated dimer –> Consider PE, image accordingly.
- Consider a TEG –> A small study looking at thromboelastography (TEG) in COVID-19 patients found that decreased clot lysis or “fibrinolysis shutdown” was associated with venous thromboembolic events, stroke and renal failure (6)
- ECMO –> consider in patients with refractory hypoxemia or cardiogenic shock. Benefit is unknown at this time (7)
Other issues
Lets talk D-Dimer –> Dimer > 2500ng/ml associated with increased thrombotic conditions and overall worse prognosis. you can read more about microvascular thrombosis, and the D-Dimer here: https://meyeringmethod.com/hypercoagulability-heparins-and-the-d-dimer-in-covid-19/
Nebulized breathing treatments such as albuterol in theory carry a higher risk of aerosolized transmission however viral transmission from this method showed conflicting results (8). Consider MDI treatments where indicated as first line. (9)
We have been asked by our clinical pharmacists to avoid Azithromycin for bacterial pneumonia. Use Doxycycline + Ceftriaxone instead of the previous recommendation of Azithromycin + Ceftriaxone. Reasons for the change: If the patient is later identified as COVID +, the inpatient team often initiates Hydroxychloroquine. Combination of Hydroxychloroquine and Azithromycin can have deleterious cardiac effects. Azithromycin has a long half-life (60-72 hours) therefore these cardiac effects can be prolonged.
NSAIDS have been speculated as causing worsening or prolonged course but there is no current data. Clinicians are recommending acetaminophen as first line antipyretics. (10).
Pediatric cases appear rarer and are typically less severe (11). There is a rare phenomenon seen termed “Multisystem inflammatory syndrome in children (MIS-C)”. Cases seen thus far resembled Toxic shock, cardiogenic shock ie myocarditis and possible vasculitis-like illness similar to kawasakis (12). There is no clear best treatment in this scenario.
There is limited data on pregnant and/or breastfeeding patients with COVID-19. A report from NEJM noted no increase in severity or increased risk of pregnancy related complications from COVID-19 in pregnant patients. (13). A study evaluated a small sample size of breastfeeding patients and noted no vertical transmission with breastfeeding.(14)
Proposed respiratory management algorithm
Read more about COVID management from EMRAP’s CorePendium Here: https://www.emrap.org/corependium/chapter/rec906m1mD6SRH9np/Novel-Coronavirus-2019-COVID-19?MainSearch=%22covid%22&SearchType=%22text%22#h.nuqesmnnl9l
References
- Lavezzo, E., Franchin, E., Ciavarella, C., et al. Suppression of COVID-19 outbreak in the municipality of Vo, Italy Doi:https://doi.org/10.1101/2020.04.17.20053157. Available April 18, 2020. Accessed April 18, 2020.
- Wang D, Hu B, Hu C, et al. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China [published online ahead of print, 2020 Feb 7]. JAMA. 2020;10.1001/jama.2020.1585. doi:10.1001/jama.2020.1585
- https://www.emrap.org/corependium/chapter/rec906m1mD6SRH9np/Novel-Coronavirus-2019-COVID-19?MainSearch=%22covid%22&SearchType=%22text%22#h.one9yqo8hqk
- Zhu X, Ge Y, Wu T, et al. Co-infection with respiratory pathogens among COVID-2019 cases [published online ahead of print, 2020 May 11]. Virus Res. 2020;285:198005. doi:10.1016/j.virusres.2020.198005
- Mahmud E, Dauerman HL, Welt FG, et al. Management of Acute Myocardial Infarction During the COVID-19 Pandemic [published online ahead of print, 2020 Apr 21]. J Am Coll Cardiol. 2020;S0735-1097(20)35026-9. doi:10.1016/j.jacc.2020.04.039
- Wright FL, Vogler TO, Moore EE, et al. Fibrinolysis Shutdown Correlates to Thromboembolic Events in Severe COVID-19 Infection [published online ahead of print, 2020 May 15]. J Am Coll Surg. 2020;S1072-7515(20)30400-2. doi:10.1016/j.jamcollsurg.2020.05.007
- MacLaren G, Fisher D, Brodie D. Preparing for the Most Critically Ill Patients With COVID-19: The Potential Role of Extracorporeal Membrane Oxygenation [published online ahead of print, 2020 Feb 19]. JAMA. 2020;10.1001/jama.2020.2342. doi:10.1001/jama.2020.2342
- Tran K, Cimon K, Severn M, Pessoa-Silva CL, Conly J. Aerosol generating procedures and risk of transmission of acute respiratory infections to healthcare workers: a systematic review. PLoS One. 2012;7(4):e35797. doi:10.1371/journal.pone.0035797
- Coronavirus disease 2019. American Society of Health-System Pharmacists. https://www.ashp.org/Pharmacy-Practice/Resource-Centers/Coronavirus.
- Little P, Moore M, Kelly J, et al. Ibuprofen, paracetamol, and steam for patients with respiratory tract infections in primary care: pragmatic randomised factorial trial. BMJ. 2013;347:f6041. Published 2013 Oct 25. doi:10.1136/bmj.f6041
- Dong Y, Mo X, Hu Y, et al. Epidemiological Characteristics of 2143 Pediatric Patients With 2019 Coronavirus Disease in China [published online ahead of print, 2020 Mar 16]. Pediatrics. 2020;e20200702. doi:10.1542/peds.2020-0702
- DeBiasi RL, Song X, Delaney M, et al. Severe COVID-19 in Children and Young Adults in the Washington, DC Metropolitan Region [published online ahead of print, 2020 May 13]. J Pediatr. 2020;10.1016/j.jpeds.2020.05.007. doi:10.1016/j.jpeds.2020.05.007
- The New England Journal of Medicine Website. Clinical Characteristics of Pregnant Women with Covid-19 in Wuhan, China. DOI: 10.1056/NEJMc2009226. https://www.nejm.org/doi/full/10.1056/NEJMc2009226?query=featured_home.
- Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. Science Direct website. https://www.sciencedirect.com/science/article/pii/S0140673620303603.
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7171388/
- Weinstock MB, Echenique A, Dabr JW, et al. Chest X-Ray Findings in 636 Ambulatory Patients with COVID-19 Presenting to an Urgent Care Center: A Normal Chest X-Ray Is no Guarantee. https://www.researchgate.net/profile/Ana_Echenique3/publication/340608073_Chest_X-Ray_Findings_in_636_Ambulatory_Patients_with_COVID-19_Presenting_to_an_Urgent_Care_Center_A_Normal_Chest_X-Ray_Is_no_Guarantee/links/5e94987f4585150839dadaf6/Chest-X-Ray-Findings-in-636-Ambulatory-Patients-with-COVID-19-Presenting-to-an-Urgent-Care-Center-A-Normal-Chest-X-Ray-Is-no-Guarantee.pdf.
- Wax RS, Christian MD. Practical recommendations for critical care and anesthesiology teams caring for novel coronavirus (2019-nCoV) patients [published online ahead of print, 2020 Feb 12]. Directives concrètes à l’intention des équipes de soins intensifs et d’anesthésiologie prenant soin de patients atteints du coronavirus 2019-nCoV [published online ahead of print, 2020 Feb 12]. Can J Anaesth. 2020;10.1007/s12630-020-01591-x. doi:10.1007/s12630-020-01591-x
- Paranjpe I, Fuster V, Lala A, et al. Association of Treatment Dose Anticoagulation with In-Hospital Survival Among Hospitalized Patients with Covid-19. JACC pre-print. 2020 May. http://www.onlinejacc.org/content/early/2020/05/05/j.jacc.2020.05.001?_ga=2.43975782.2106321362.1588867415-203472150.1583280090
- Lippi G, Plebani M. Laboratory abnormalities in patients with COVID-2019 infection [published online ahead of print, 2020 Mar 3]. Clin Chem Lab Med. 2020;/j/cclm.ahead-of-print/cclm-2020-0198/cclm-2020-0198.xml. doi:10.1515/cclm-2020-0198
- Lauer SA, Grantz KH, Bi Q, et al. The Incubation Period of Coronavirus Disease 2019 (COVID-19) From Publicly Reported Confirmed Cases: Estimation and Application [published online ahead of print, 2020 Mar 10]. Ann Intern Med. 2020;10.7326/M20-0504. doi:10.7326/M20-0504



This Post Has 0 Comments