**Updated 4/15**
We have been seeing reports of patients that have been presenting awake, nont altered or obtunded, in moderate respiratory distress, tachypnea, but without gross signs of central or peripheral cyanosis with SPO2 <70%. As per some social media updates and trends, this has been now dubbed “silent hypoxemia”.(1)
Personally I have seen this so far about 15 times in the past 3 weeks in patients with presumed COVID. Several of these patients received a workup for PE however in all cases CTPA was negative, and showed the infiltrative process we have come to associate with typical COVID infection by CT imaging. Anecdotally I placed all of these patients on NC/HFNC/NRB 6-15L for about 30 min -2 hrs with repositioning (make the patient lie prone 30 min, then on each side x30 mins and repeat) and they had no mental status changes and no progressive increased dyspnea or decompensation, actually they progressed rapidly in about 30 minutes and were improving clinically. SPO2’s ran about 90-93% at that point. I think this has relatively saved them from an intubation early, and several of these patients did not end up needing intubation later in the hospital course.
Some initial COVID data coming from Italy – suggesting using BRESCIA scoring to determine intubation. This has been a point of contention amongst US front line physicians (6).
This brings us to the recent postulations that we should probably try to defer intubation on some of these patients and treat the patient as a whole instead of treating the pulse ox number (ie factoring in mental status etc), as for now we are dealing with a new norm (1,2,5).
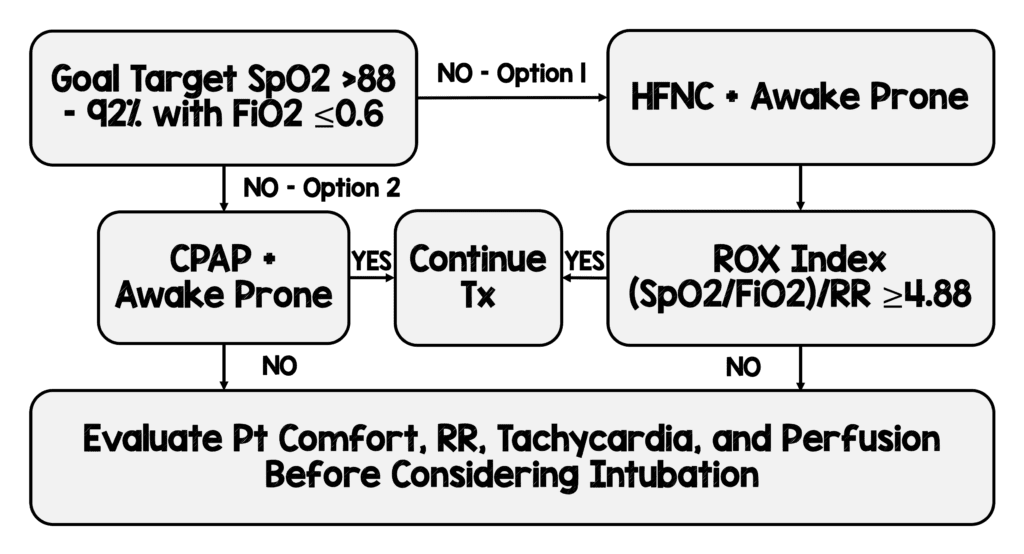
REBELEM has suggested the following protocol and approach to those in minimal to moderate respiratory insufficiency. (See below)
There is also a great article about how much air dispersion is actually created with NC and HFNC, and what the impact of putting a simple surgical facemask on these patients on NC would accomplish:
The TL;DR version of this is essentially as follows: With the use of a surgical mask (Not N95) on the patient overtop NC or HFNC, there should be minimal aerosolization <1 meter from the patient. This in theory should show that there is less aerosolization than previously thought once precautions are utilized – as opposed to strict airway control with ETT/intubation.
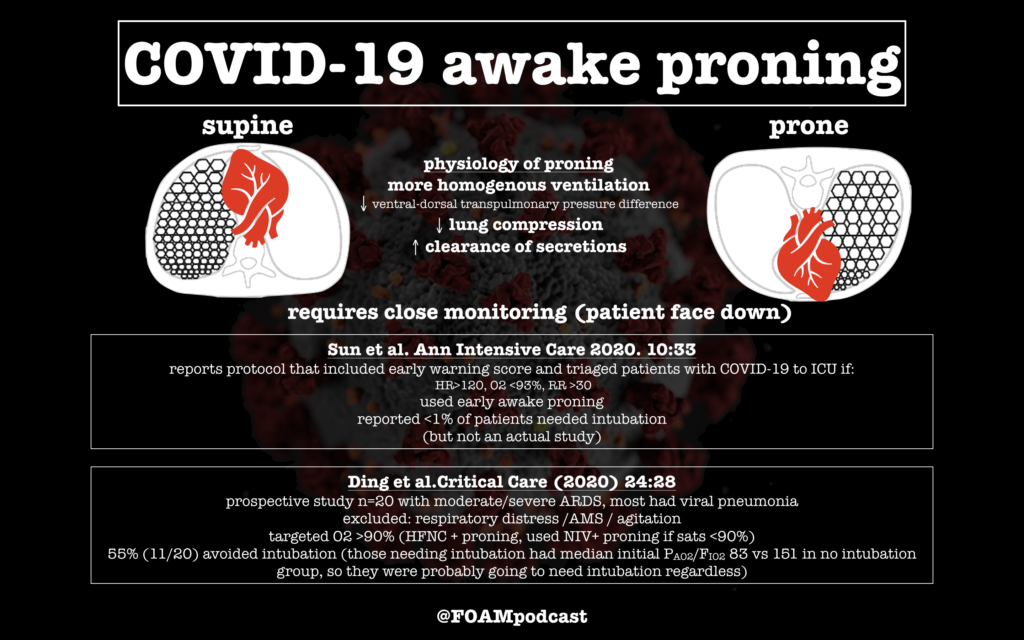
How about awake proning? Annals of intensive care published an article addressing exactly this which came out on 3/18/2020. It was also reiterated by FOAMCast as below. In both studies the rate of intubation was <1%, and in the Ding et al. study 55% (11/20) actually avoided intubation. (7) We should probably perform more awake proning and positioning of patients early, become more comfortable with some SPO2 low numbers – assuming the patient is able to tolerate – and try some recruitment measures or alterations of pulmonary flow measures with these techniques.
What we do know is that mechanical ventilation seems to cause destruction on the respiratory system in COVID-19 patients with very high mortality from all sources (Variable 67%-88% mortality for ALL intubated patients regardless of initial respiratory severity). If we can avoid “early airway control” as once was initially thought superior as much as possible without compromising organ O2 delivery and neurological function, this may be a much better conservative approach prior to more invasive respiratory support measures.
References
- https://rebelem.com/covid-19-hypoxemia-a-better-and-still-safe-way/
- Ding L et al. Efficacy and Safety of Early Prone Positioning Combined with HFNC or NIV in Moderate to Severe ARDS: A Multi-Center Prospective Cohort Study. Crit Care 2020. [Epub Ahead of Print]
- Munshi L et al. Prone Position for Acute Respiratory Distress Syndrome. A Systematic Review and Meta-Analysis. Ann Am Thorac Soc 2017. PMID: 29068269
- Clinical management of severe acute respiratory infection when novel coronavirus (2019-nCoV) infection is suspected: Interim Guide, January 28 2020.
- Leung CCH, Joynt GM, Gomersall CD, et al. Comparison of high-flow nasal canula versus oxygen face mask for environmental bacterial pneumonia patients, a randomized controlled crossover trial. J Hosp Infect 2019: 101:84-87.
- https://www.acep.org/corona/search-redirects/italian-guidelines-for-covid-19/
- https://annalsofintensivecare.springeropen.com/articles/10.1186/s13613-020-00650-2